Our initial fear of COVID-19 infection was of becoming seriously ill, ending up in hospital and possibly even dying. Through each of the three waves of infection, the pressure of infected patients filling hospitals and scarce ICU beds led to a marked reduction in non-emergency care even for serious need.
As infection rates drop dramatically more than 70 percent of Canadians over age 12 receiving at least one jab and nearly 20 percent being fully vaccinated to date what do we still have to worry about?
The Delta variant, recognized in India, appears to be more resistant to a single vaccination dose. That means it is essential that high risk people — those over 60 or with obesity, diabetes and immune-compromised conditions — receive priority for second shots. They also need to be encouraged to do so through ease of bookings and increased efforts to overcome any residual vaccine hesitancy.
Getting a second shot for as many people as possible remains essential to keeping case rates and hospitalizations low. In order to achieve relative herd immunity we hope that over 80 percent of people eligible for vaccination will be fully covered by the end of summer. Canada has a very large vaccine supply coming in the next two months making timely second shots readily available.
The burden of getting COVID-19 goes beyond the initial effects of infection. We now know that there can be very significant long term effects that can persist for months or longer. The syndrome is know as “long COVID“ or “long-haul COVID.”
COVID-19 infection can involve multiple organ systems including the lungs, heart, brain and kidneys. This is a result both of direct infection and a potential over-reaction of the body’s natural immune response. While most people who are infected resolve symptoms within 2 weeks, there is a growing body of scientific literature that characterizes the nature and duration of persisting symptoms.
The diagram below from emergency-live.com highlights the organ systems that COVID-19 infection targets with potential long-lasting impact. Possible mechanisms include prolonged inflammatory response, nerve damage, retained viral load and blood clotting problems. There is also a major psychological effect to being severely ill with potential long term mental health consequences.
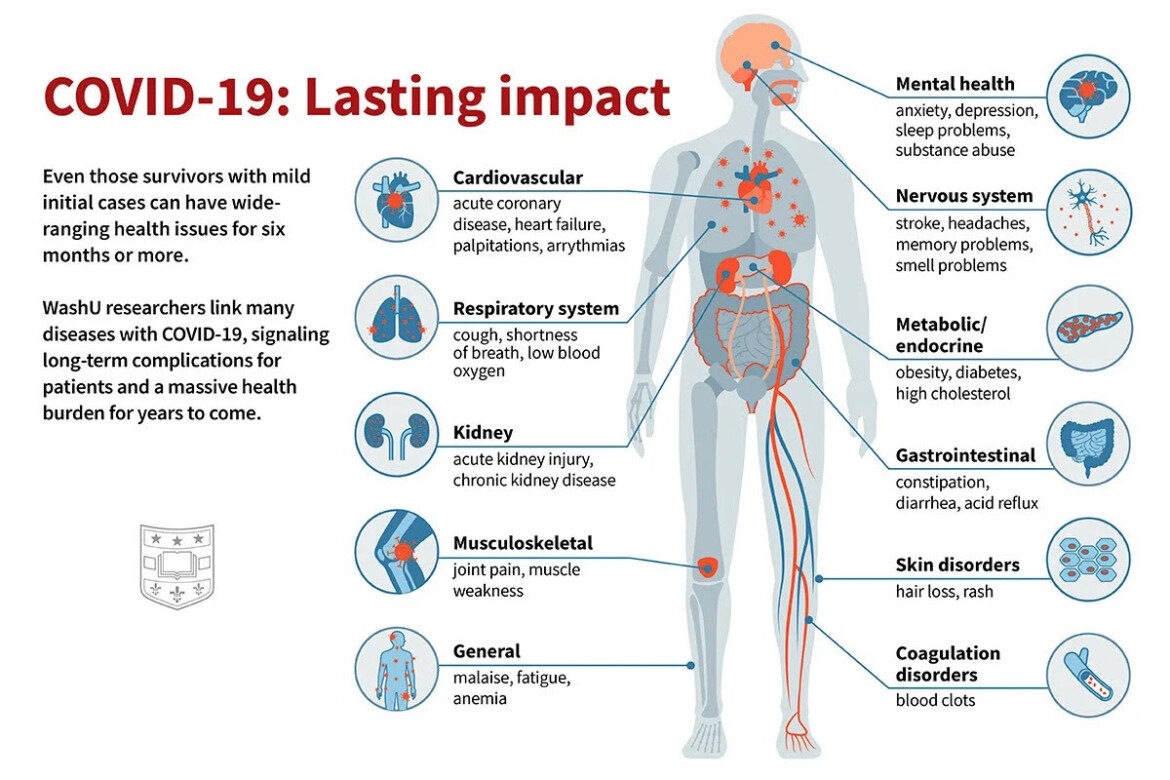
The lungs are a prime target of infection. While COVID pneumonia generally clears early, a small number of patients may have lingering scarring that may be permanent and can reduce lung function with persisting shortness of breath. Others may have blood clots leading to strokes, kidney damage or small blood vessel blockage and lingering disability as a result.
A large United States Department of Veterans Affairs study showed a 60 percent increase in all cause mortality within six months of infection especially if hospitalization was necessary.
In a Swedish study of infected health care professionals, 80 percent of hospitalized patients experienced moderate to severe symptoms for many months after initial infection and 10 percent of all those infected, but not hospitalized, experienced one or more moderate to severe symptoms affecting quality of life for more than six months.
A common specific symptom of infection is loss of smell and taste. While not life-threatening, it is very challenging to many and may greatly affect quality of life. The virus does not appear to directly damage the nerve cells that allow us to smell and taste but rather their supporting cells. While these sensory losses may persist for two months after infection in about 25 percent of affected people and in 15 percent beyond eight months, function will ultimately recover in most people.
The virus also affects brain function, perhaps by causing an inflammatory reaction. This can result in persisting brain fog with difficulty concentrating and memory impairment, as well as anxiety and depression.
Chronic fatigue is a known major complication of some viral infections especially mononucleosis and is a significant long-COVID symptom as well. Many patients describe a persisting inability to work or function at a high level.
Vaccine hesitancy has been increased by the belief that healthy people who get infected will only feel like they got the flu. However, it is important to remember that even those with mild symptoms may develop long-haul COVID symptoms, which can be debilitating.
It is estimated that about 20 million people worldwide will develop long-haul COVID symptoms. We don’t yet know who is most at risk other than by the severity of infection. Unfortunately there is no effective treatment to date.
Physicians and patients need to respect that unusual and persisting symptoms after infection are real even when conventional testing fails to reveal blood or imaging abnormalities.
If you are young and healthy and, as a result, vaccine hesitant, preventing long-haul COVID is another good reason to get fully vaccinated as soon as possible.
Recommended for You

Daniel Zekveld: Age verification for pornography is not government overreach

Colin Craig: A roadmap to more choice in health care

Canada outperforms the U.S. on many well-being measures—yet on the important economic indicators, we are falling far behind

‘Enormously expensive and very narrow’: Kevin Quigley on Canada’s precautionary response to COVID-19



