What is the plan?
This is the question we should be asking ourselves morning, noon, and night.
Ontario and Quebec, the economic engines of the nation, cannot endure another COVID shutdown. Shaky public finances will buckle. Public confidence will collapse. Talent will flee. An already acute physical and mental health crisis will metastasize into a tragedy of unimaginable suffering. It is by no means hyperbole to posit that the risk of another prolonged shutdown is existential.
Yet here we find ourselves again…slowly and painfully emerging from the fourth round of mass closures in twenty months with not only no plan in sight but the absence of even a discussion of what we could do to prevent future shutdowns.
Who is to blame for the void of ideas and action on the single most important issue we face? It’s too easy to call out hyperreactive politicians and governments. Both are in survival mode caught up in case counts, hospitalizations, and polling numbers. The media sadly has shown itself to be largely uninterested in examining the hard choices required to pandemic proof our institutions. Instead, clickbait COVID headlines and “hot takes” from the country’s self-appointed COVID expert class clog our social feeds and desktops. The result is we are two years into this crisis and have yet to have any kind of coherent conversation about the steps and actions we need to take to avoid a fifth, sixth, or seventh lockdown.
The real culprit of our collective inaction and paralysis is us. It’s the broad public who are deeply uncomfortable with the difficult truths COVID-19 has revealed about our single most important and cherished public institution: health care.
Public health care systems were in trouble before the pandemic. We knew we were rationing care through the silent suffering of lengthy wait times. We knew the opioid epidemic was, in part, a reflection of systems that lacked the resources to address chronic illness and debilitating pain. We knew that the delivery of health care had become overly bureaucratized. But despite all these failings we clung to our single-payer system because it represented one of the last vestiges of an older civic compact based on an ethos of mutual care and solidarity.
The pandemic has done something more pernicious to public health care than just flooding our hospitals with sick and dying, canceling lifesaving surgeries, and burning out legions of frontline workers. It has turned a touchstone of common identity into the foil for our collective immiseration through shutdowns, closures, restrictions on basic civil liberties, and divisive debates about vaccines.
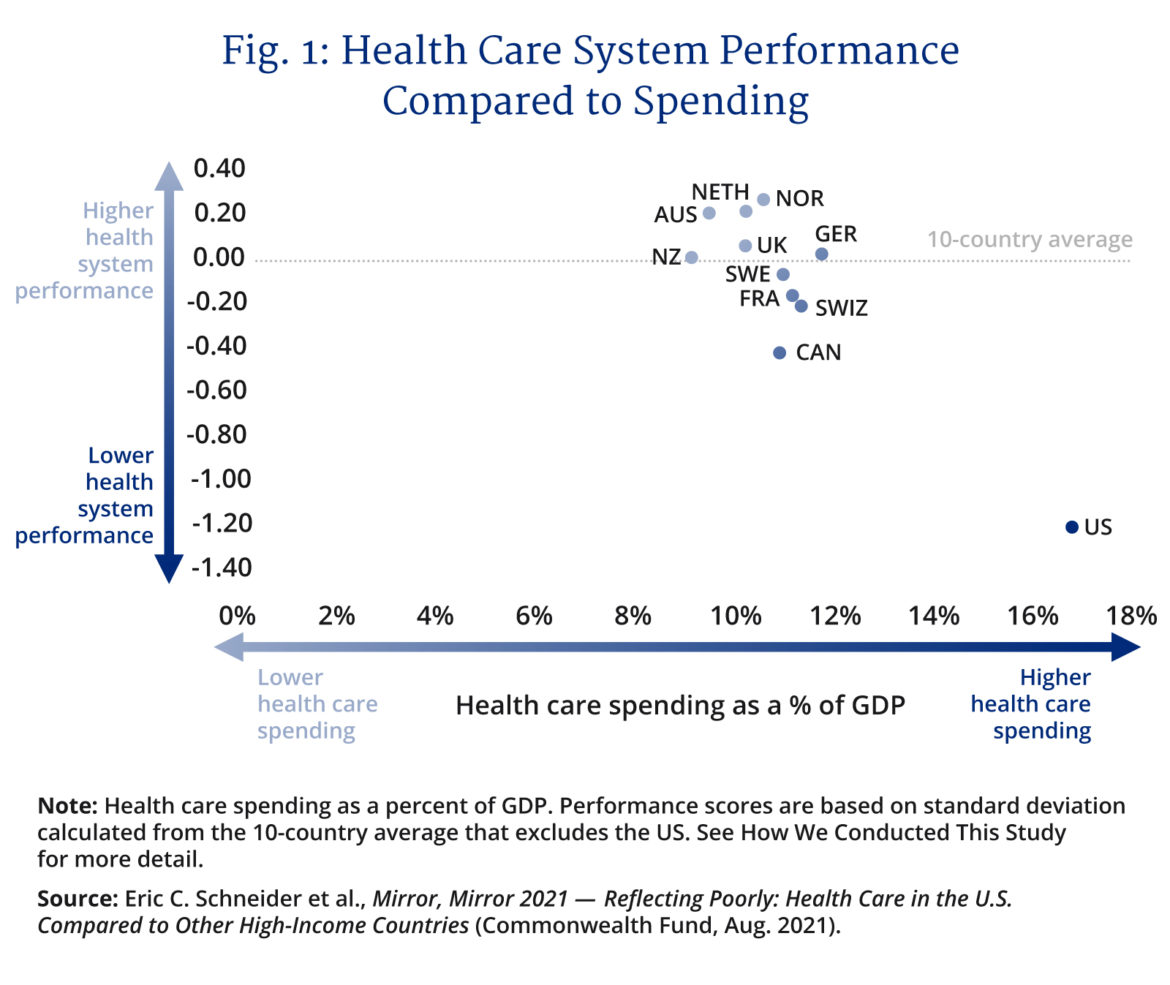
With fewer intensive care units per 100,000 people than Mongolia and total bed capacity near the bottom of the OECD, our public health systems have become choke points that strangle any effective, long-term strategy to manage COVID-19.
How else do you explain a province like Ontario with almost 15,000,000 residents repeatedly shutting down when its COVID-related critical care admissions top four hundred, or a paltry one I.C.U. COVID patient for every 40,000 residents?
This we know: there will be more variants. Some will be milder than Omicron. Some less infectious. Others may not. With billions of people around the world unvaccinated and immunocompromised, COVID will mutate relentlessly looking for new ways to evade both vaccines and naturally acquired immunity. The comforting prediction that COVID will soon become endemic and mostly harmless is an assumption based on past pandemics shaped by different pathogens, different public health responses, and different therapeutic technologies (e.g. there weren’t tens of millions of people on retroviral drugs in 1918-19). The risk of future shutdowns in a significantly health care-constrained country such as Canada isn’t some hazy hypothetical, it’s a highly probable event in our near-term future.
We are at the breaking point. The debilitating effects of another shutdown cannot be overstated. As painful and disorienting as it will be for our collective sense of self, we have to rethink health care delivery. Everything needs to be on the table, from the private funding of the medically necessary hospital and physician costs, to public/private partnerships to build more hospitals, to opening up professional credentialization, to user fees, to the holy of holies: a rethink of universality itself.
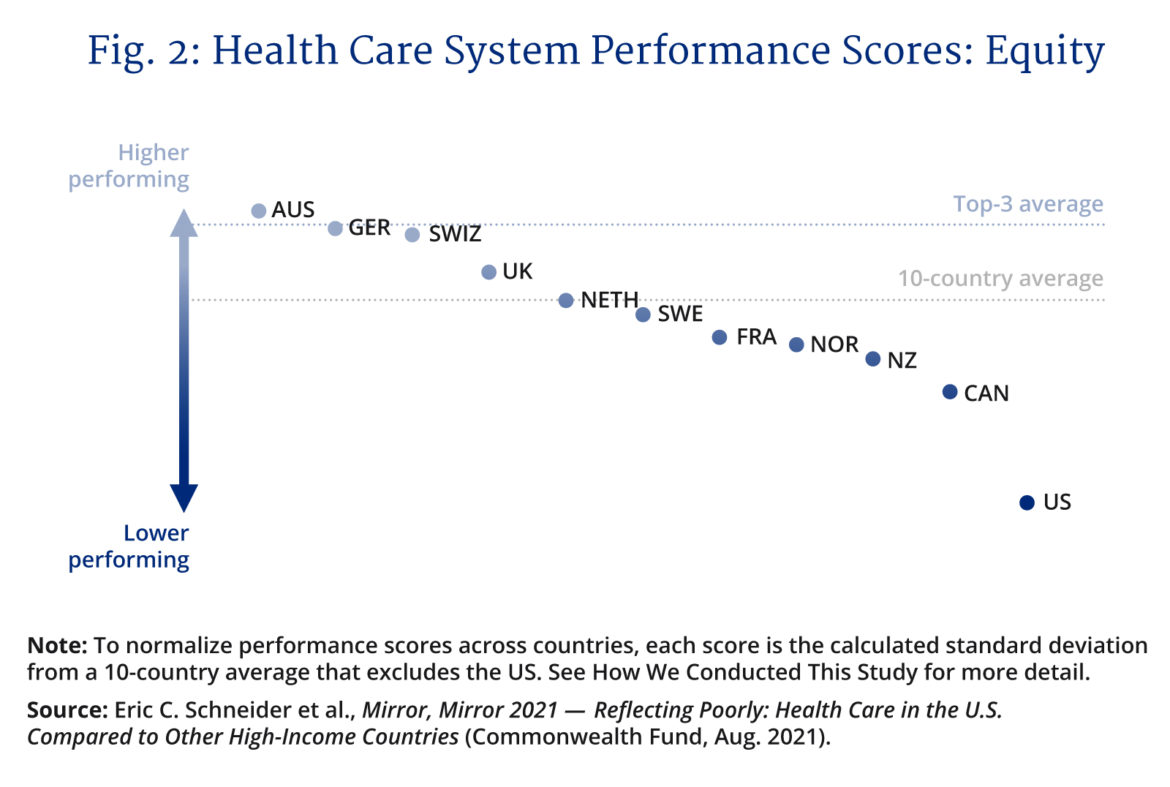
Fortunately, we can learn from countries that are much farther down the road of health care innovation and reform and who have efficient and high-performing health care systems such as Norway, the Netherlands, and Israel, to name a few. Systems that proved themselves better able to cope with the surges in infection that have swept the world repeatedly and will do so for the foreseeable future. We need to follow their tracks and move fast. The virus isn’t waiting. It’s mutating.
The rejoinder to such a clarion call is to increase government funding and build more hospitals, hire more doctors and nurses, expand not contract universality to pharma care, dental care, etc., etc., etc. We are in an emergency. The clock on the next shutdown is ticking. With most provincial budgets already allocating 40 percent or more of revenues to health care, there aren’t the resources to do what needs to be done at the speed with which a transformation has to happen. Ottawa is similarly financially constrained as our debt-addled federal government falls ever deeper into deficit spending in the tens of billions annually for years to come.
If we want to be honest with ourselves the traditional response of injecting more government funding into health care wasn’t working before COVID. Wait times were increasing. Bureaucratization was growing. Patient outcomes were worsening. Health care costs were growing faster than inflation and population.
The problems with the current system are structural. We can only change the system and start down the road of pandemic proofing our hospitals, economy, schools, and day-to-day lives if the change itself is structural. Anything short is a copout that will set the country up for another round of debilitating shutdowns.
None of this is pleasant. No one is contemplating wrenching changes to an institution like health care that is integral to our national way of life with glee. This isn’t about ideology. It’s about facing up to reality. It’s about living with this novel virus and the threat it represents for years and possibly decades to come.
To fail in this singular task is to condemn ourselves to Einstein’s definition of insanity, doing the same thing over and over and expecting a different result.
Yet, nothing about this crisis is inevitable including future shutdowns. It’s past time to reform health care delivery in Canada and reclaim our agency in the era of COVID that will impact our way of life, like it or not, for years to come.
Recommended for You

Need to Know: Mark Carney’s digital services tax disaster

Theo Argitis: Carney is dismantling Trudeau’s tax legacy. How will he pay for his plan?

Kirk LaPointe: B.C.’s ferry fiasco is a perfectly Canadian controversy

‘I want to make Canada a freer country’: Conservative MP Andrew Lawton talks being a newbie in Parliament, patriotism, and Pierre Poilievre’s strategy




