In Canadian public policy, few subjects are as sacrosanct as the single-payer health-care model. For decades, it has been woven into our conception of national identity. It has been a defining feature that distinguishes us from our American neighbours as much as it has been a system of financing and delivery of health care. Yet, this sacred cow is now facing its most significant challenge in a generation.
The government of Alberta, under Premier Danielle Smith, is reportedly poised to introduce legislation that would fundamentally alter this landscape. According to reports, the proposed reforms would permit the establishment of a parallel private health-care system, allowing doctors to work within both the public insurance model and a for-profit delivery system. If these reports are accurate, this represents not merely a provincial policy shift, but one of the most consequential health-care reforms in Canadian history.
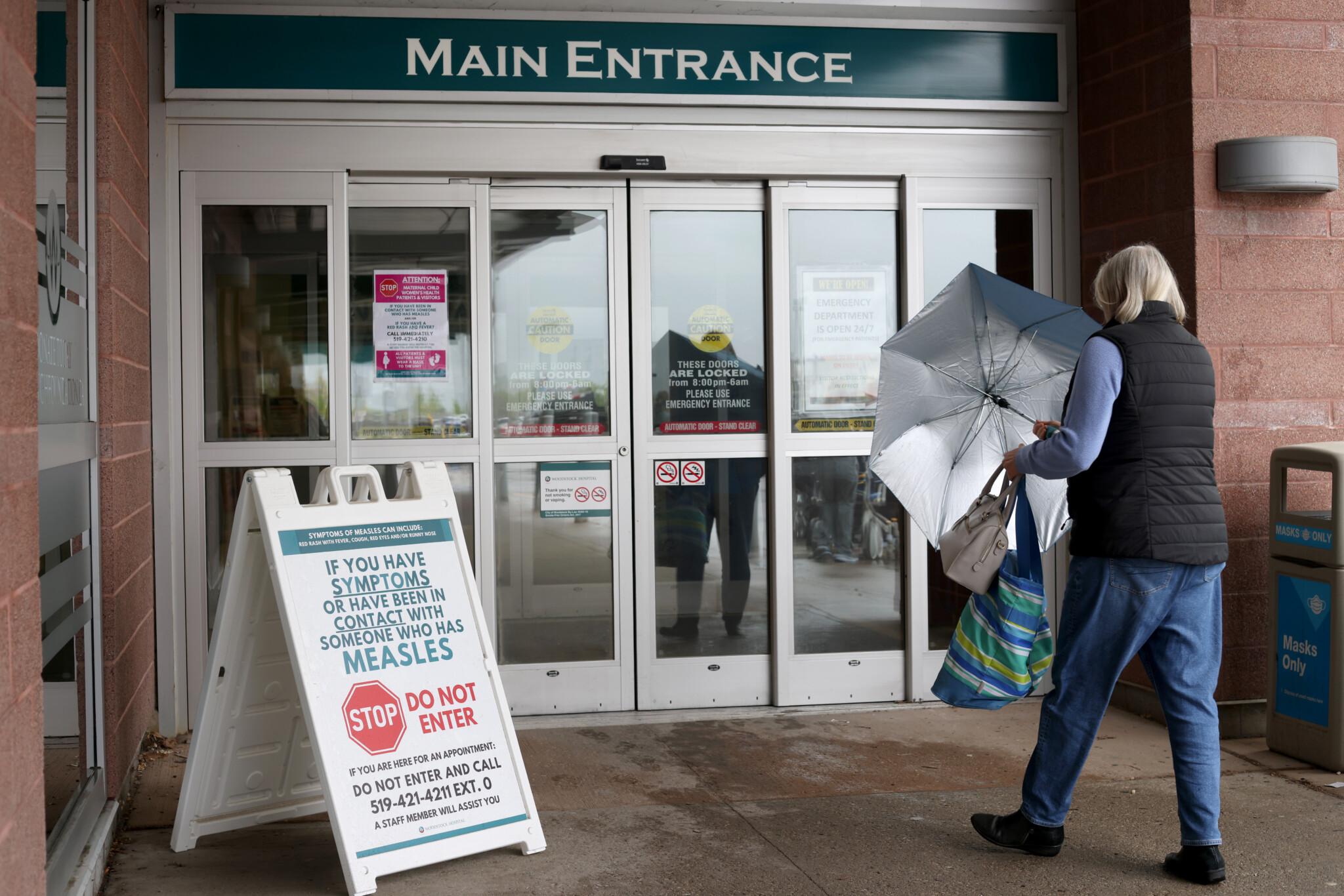
Why is this development sending shockwaves through the country? Because it directly confronts a monolithic system that, for all its symbolic power, is showing profound signs of failure. The evidence of crisis is mounting, and it’s no longer just about long wait times. We regularly confront stories of patients with advanced-stage cancer being sent home without treatment plans, overflowing emergency rooms, and the near impossibility of finding a family doctor for millions of Canadians. The rationing inherent in the current model is causing real pain, suffering, and, in tragic cases, preventable death.
Furthermore, the fiscal burden is unsustainable. In many provinces, health care consumes between 30 and 40 percent of all program spending. This massive allocation starves other critical priorities—from higher education and infrastructure to social services. The status quo, in other words, is a health-care crisis; it is a millstone around the neck of our entire public sector and the economy broadly.
The reflexive counterargument from defenders of the single-payer system is often rooted in a commendable egalitarianism—the principle that access to care shouldn’t depend on one’s ability to pay. We share this principle.
Universality is a noble goal. However, the current reality is a perversion of this ideal. The system isn’t fully universal if it fails to deliver timely care. Moreover, a two-tier system already exists de facto for those with the means to travel to the United States or other provinces for treatment. Our current model creates a paradox where egalitarianism denies timely care to everyone, while the wealthy find a way out.
Alberta’s proposed model, as we understand it, isn’t an adoption of American-style health care. It looks far more like the mixed systems common throughout Europe—societies often lauded for their progressivism. In these countries, the integration of private capital and delivery, often with mandates for physician time in the public system, complements public health outcomes. Canada finds itself in a shrinking group of holdouts, including the likes of the failing NHS in the U.K. and its Italian equivalent, in its dogmatic adherence to a single-payer monopoly.
A significant impediment to such reform has always been the federal Canada Health Act. This statute sets out principles provinces must follow to receive their full federal health transfers. Alberta’s legislation will almost certainly be offside, potentially jeopardizing its $6 billion annual health transfer from Ottawa. This sets the stage for a major federal-provincial confrontation, arriving ironically at a moment when cooperation between Ottawa and Alberta on other issues, like pipelines, seems to be growing.
This political fight, however, shouldn’t obscure the core necessity of experimentation. The basic premise of our federation is that it allows for provincial laboratories of policy innovation. Alberta is poised to become a crucial incubator for health-care reform. If its model succeeds in increasing the supply of health services, reducing wait times, attracting medical professionals, and improving outcomes without sacrificing equity, it will create competitive pressure on other provinces to follow suit. If it fails, it will offer valuable lessons.
The current one-size-fits-all approach across Canada’s provinces has resulted in uniformly poor performance. Doing the same thing over and over while expecting a different result is, as Einstein noted, the definition of insanity.
We at The Hub believe that issues of fairness and equity must be central to any reform. The details of the Alberta legislation will be paramount. But the simple defense of the status quo is a denial of a multifactorial reality. The single-payer system is broken, and the need for structural change is urgent.
Alberta’s gamble is a bold embrace of federalism’s potential. We hope that Ottawa, despite inevitable pressure to intervene and penalize the province, will resist. Allowing provinces to experiment is how we progress. In no area is this innovation more desperately needed than in health care. In goring this sacred cow, Alberta is attempting to lead the herd out of a crisis. For the sake of all Canadians, we should watch, learn, and hope it succeeds.
This commentary draws on a Hub podcast. It was edited using AI. Full program here.
Alberta's health reform: Is a parallel private system the disruption needed, or a step towards privatization?
Will Alberta's health reforms trigger a federal-provincial showdown over funding?
If Alberta's health experiment fails, what are the potential lessons for Canada's healthcare?








Comments (2)
I’m looking forward to the critics of the changes Danielle Smith is planning. It will be a carnival of spurious arguments and hysteria from the Regressives. Only in Canada.