The Hub’s first annual Hunter Prize for Public Policy, generously supported by the Hunter Family Foundation, focused on solving the problem of long wait times in Canada’s health-care system. A diverse group of ten finalists have been chosen from nearly 200 entries, with the finalists and winners chosen by an esteemed panel of judges, including Robert Asselin, Dr. Adam Kassam, Amanda Lang, Karen Restoule, and Trevor Tombe. The Hub is pleased to run essays from each finalist this week that lay out their plans to help solve this persistent policy problem. The winners of the first-ever Hunter Prize for Public Policy will be announced on Friday, September 29.
The Canadian health-care system is a collection of provincial and territorial health-care systems, all of which are struggling with long wait times and the risks this poses to patients, health-care providers, and quality of care in the long term. While long wait times are nothing new to Canadians —a staggering 55 percent of whom can’t find a family doctor or have difficulty accessing one—this problem isn’t going away as wait times are increasing and Canada is falling further behind its peer countries.

The consequences of long wait times have been well documented and include negative health outcomes, patient stress, worsening medical conditions, increased long-term health costs, and declining trust in the health-care system. Couple this with the fact that wait times impact Canadians disproportionately, with low-income individuals waiting longer for health services than their high-income counterparts, it’s time for policymakers to consider implementing a solution hidden in plain sight: Canada’s supply of internationally trained health-care providers sitting on the sidelines.
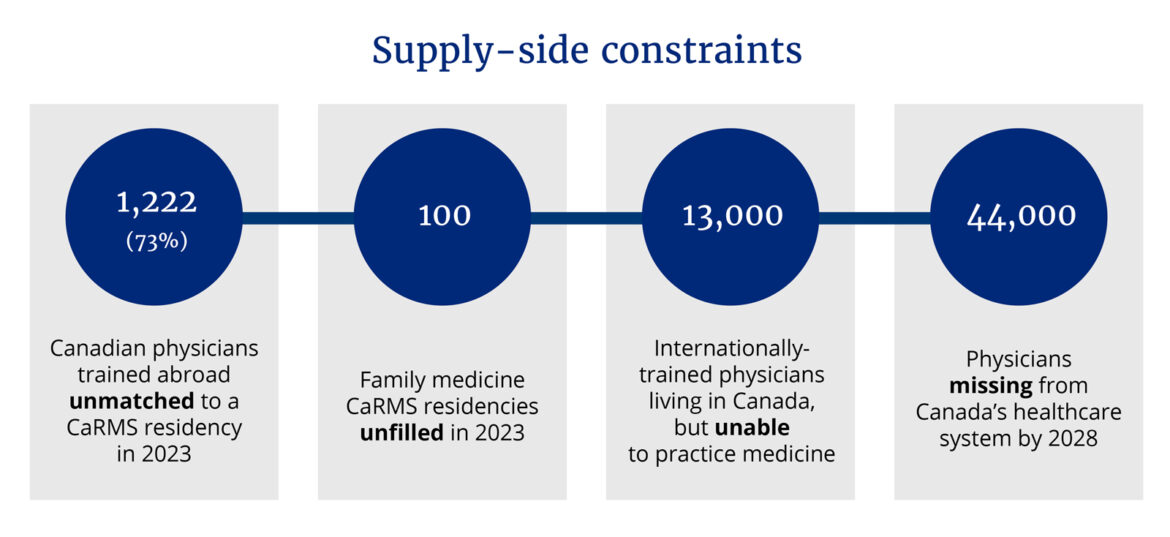
There are thousands of Canadians who trained abroad at international medical schools and permanent residents who have previous experience as doctors but who are left out of the health-care system due to regulatory barriers and limited residency spots, something required before doctors can practice. In 2023, among 1,661 Canadian physicians trained abroad, only 439 (or 27 percent) were matched to a post-graduate residency. Among physicians starting their residency, the popularity of family medicine is also falling, with a drop in first-choice ranking from 35 percent in 2013 to 30 percent in 2023 among Canadian medical graduates. Further, while only 33 family medicine residencies went unfilled in 2019, this number rose to 100 in 2023.
While family medicine positions remain unfilled and up to six million Canadians are without a doctor, there are an estimated 13,000 internationally-trained doctors living in Canada, many of whom have received permanent resident status, but who are unable to work in the health-care sector due to regulatory barriers. This untapped surplus of trained health-care professionals is particularly worrying given the shortage of family doctors in Canada, such that 20 percent of Canadians are without regular access to a primary care provider, with an expected shortage of nearly 44,000 physicians by 2028.
A simple, feasible, and effective option would be for provincial regulatory bodies (Colleges of Physicians and Surgeons) to pilot a new licensing option for internationally trained health-care providers (ITHPs). Eligible ITHPs would include Canadians trained at select foreign medical schools and foreign nationals already in Canada who hold medical degrees from select institutions. This regulatory license would include a low-risk, limited scope of practice that meets the demands of primary-care services while mobilizing the untapped supply of trained health-care providers, all while preserving provinces’ existing regulatory landscape and the trust that Canadians have in existing titles (e.g., nurses/doctors) and the broader health-care system.
The ITHP license would not be commensurate with that of doctors but would instead include a limited scope of practice that bridges the supply-side surplus with the demand-side shortcomings, such that ITHPs can take on primary care roles in family physician clinics, ambulatory care settings, community health centres, long-term care homes, and other lower-risk settings, as determined by each province. This policy could bring in previously “unmatched” internationally-trained medical graduates who did not complete their residency, effectively leveraging the training and expertise of an initial more than 1,200 ITHPs at the outset.
The feasibility of this option is highlighted by the fact that it is provincially led. While some calls to nationalize or create pan-Canadian portals or triage systems have gained popularity, the reality is that provinces have jurisdiction over health care and are unwilling to relinquish this constitutional responsibility. Though funded in part by the per-capita-based Canada Health Transfer from Ottawa, provinces administer their own health-care systems, including public health insurance programs and regulatory bodies for doctors and nurses. The result is a complex series of provincial health-care systems with different billing procedures, rules, licenses, and funding. Instead of pushing for greater involvement from Ottawa or national models, policymakers should recognize that realistic solutions have to be led by and attuned to the unique contextual needs of each province.
With provinces leading the creation of this new license for ITHPs, no new regulatory colleges would be required, which would limit cost duplication, ensure compliance with existing limits, and provide contingency planning where provinces could opt to sunset this pilot program. Further, ITHPs would be integrated into existing provincial health plans such that billing practices match those already in place. The ability of the policy solution to be integrated within existing provincial health-care institutions lends itself to low costs, political feasibility, and ease of evaluation in both the short- and medium-term.
Though long wait times sometimes bring about calls for AI-generated solutions and virtual care clinics, the reality is that Canadians are not looking for techno-health innovation the way that bureaucrats and software engineers might assume; they just want to be able to see a doctor. Canadians should not be forced to accept lower-quality health-care services such as long wait times or virtual substitutes. Instead, it is policymakers who should bridge the gap by recognizing the skills of Canada’s untapped supply of internationally-trained healthcare providers; the health of Canadians and our provincial health-care systems depends on it.




