The Hub’s first annual Hunter Prize for Public Policy, generously supported by the Hunter Family Foundation, focused on solving the problem of long wait times in Canada’s health-care system. A diverse group of ten finalists were chosen from nearly 200 entries, with the finalists and winners chosen by an esteemed panel of judges, including Robert Asselin, Dr. Adam Kassam, Amanda Lang, Karen Restoule, and Trevor Tombe.
Congratulations to Dr. Ashley Flanagan and Dr. Kristina Kokorelias for this $25,000 grand prize-winning proposal in the inaugural Hunter Prize. The runner-up was Bacchus Barua for a proposal arguing that changing how we fund hospitals could be the key to health-care reform.
Introduction
Successive governments across Canada have been continually challenged in effectively addressing hallway medicine and wait times for both hospital and long-term care (LTC) services. The Government of Ontario’s Ministries of Health and Long-Term Care (MHLTC) have particularly struggled to implement integrated policies and solutions, thus necessitating even greater collaboration between them to achieve a comprehensive solution.
Recognizing the need for solutions to enhance access to home and community care services as an integral component of the overall provision of LTC services in Canada, this proposal advocates for the creation of a Virtual LTC @ Home Program that aims to revolutionize the healthcare landscape.
Such a program would enable these local integrated teams of care providers (e.g., Ontario Health Teams (OHTs) and their constituent health and social care organizations) to work collectively to identify and provide a more flexible and tailored mix of care to support more LTC-eligible individuals to stay at home for as long as possible. To do so, these teams would have access to the same level of funding that would have been used to care for the same individuals in LTC homes with an aim to also tackle ever-worsening health-care waitlists and the Alternate Level of Care (ALC) crisis in Ontario – and across Canada.
The Conference Board of Canada recently estimated that to meet the growing needs for LTC services by Canada’s ageing population that Canada will need to more than double its current complement of 199,000 to 454,000 LTC beds by 2035. A Virtual LTC @ Home Program can present a more cost-effective alternative to the costly exercise of redeveloping and simply expanding the overall number of LTC beds in Ontario and across Canada, as evidenced by the case of Ontario. We feel that this proposal will clearly outline a high-impact, low-cost, politically desirable policy reform that can effectively address health care wait times and other health care delivery challenges.
Indeed, by more strongly focusing on delivering care within people’s own homes, this program has the potential to save significant capital infrastructure costs and optimize the utilization of existing LTC beds for those who need them most, while also addressing worsening issues of hallway medicine, wait times, surgical backlogs and unprecedented ALC rates that continues to plague hospitals across the country.
The Problem
Ontario’s LTC system is currently facing unprecedented capacity issues that have far-reaching consequences for the province’s overall healthcare system.
The lack of sufficient capacity to meet current demands for home and community care services have led to a record 14,000 Ontarians on its waitlists for them. Admissions into LTC homes are also becoming increasingly delayed with nearly 40,000 Ontarians currently on the waitlist – comprising 76% of the national waitlist.
This helps to explain why, as of June 30, 2023, 2,167 Ontarians, designated as ALC patients, were currently waiting in hospital beds for a bed to open up in an LTC home. ALC designations are specifically given to patients who are occupying hospital beds but no longer require care in them and could be better served in alternative care settings, such as LTC homes or with home care (HC).
As of June 30, 2023, there were 4,514 ALC-designated patients occupying 13.6% of Ontario’s hospital beds, with 48% waiting for an LTC home placement and 13% of them waiting for access to in-home care services.
At the same time, Canada—and Ontario, in particular—has one of the lowest have one of the lowest hospital bed-to-population ratios among Organization for Economic Cooperation and Development (OECD) countries (see Figure 1). This means that there are relatively fewer hospital beds available per capita compared to other countries with similar healthcare systems. In contrast, Denmark, despite also having a low hospital bed-to-population ratio, has also managed to maintain an exceptionally low ALC rate of 1%.
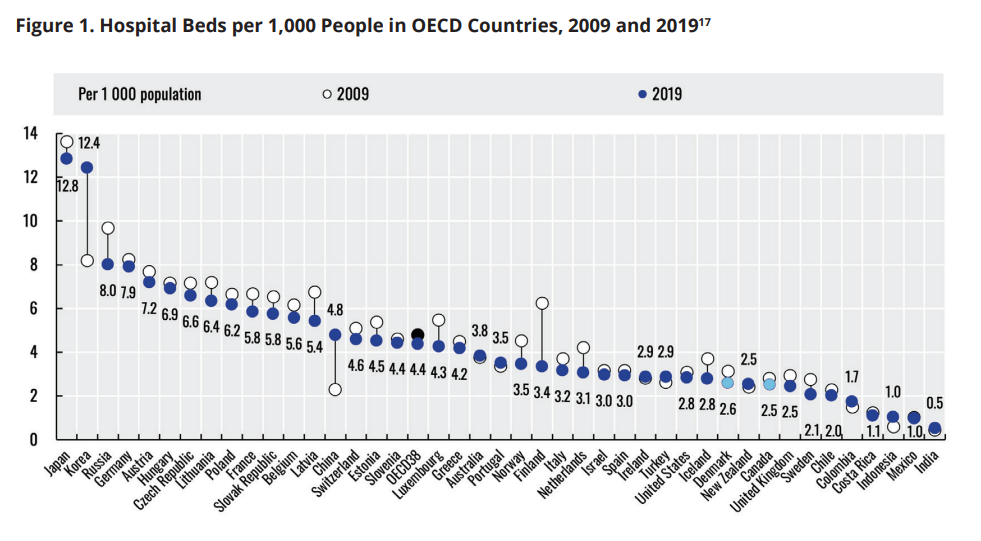
Denmark’s success in achieving a low ALC rate can be largely attributed to its strong emphasis on providing adequate HC services that allow patients to be appropriately discharged quickly from hospitals when they no longer need care in them, efficiently freeing up their hospital beds for patients in need of them. Instead, our Canadian approach has led to a domino effect which has only worsened hallway medicine and access to hospital beds with Ontarians now waiting a staggering 17.9 hours on average to be admitted to an inpatient bed from emergency departments. Limited hospital beds only serve to further delay timely access to the 206,000 Ontarians currently waiting for elective surgeries.
The COVID-19 pandemic has further prompted a massive shift in public sentiment towards a preference to remain at home for as long as possible. Overall, the capacity pressures in Ontario’s LTC system, coupled with the lack of adequate home and community care options, have profoundly impacted Ontario’s overall healthcare system, affecting timely access to care for all Ontarians and those in need of LTC services in particular.
As a result, there is a growing need for evidence-informed policy and practice solutions to address these challenges and provide better care options for Ontarians.
Current Government Initiatives
When the current Ontario government came to power in 2018, there were 32,773 individuals on LTC home waitlists and approximately 3,000 on its HC waitlists while its ALC rate encompassed 13.5% of its hospital beds. In response to these numbers, it embarked on an ambitious plan to build 30,000 net new LTC beds and renovate 30,000 older beds within 10 years at an initial estimated cost of approximately $240K per bed or $14B overall (in 2020 dollars) in related capital infrastructure construction funding subsidies – making this commitment the largest LTC building program ever launched in Canada.
From 2018 onwards, ongoing lower annual increases (when compared to the previous year) to Ontario’s HC budget have helped to see waitlists for HC services balloon to over 14,000 individuals while its LTC home waitlist has for the first time nearly topped 40,000 individuals.
Furthermore, according to Ontario’s MHLTC, in 2021-22 it supported 131,180 LTC-eligible Ontarians of all ages to live in their own homes with its existing range of available HC services. The MHLTC further estimated that the HC costs to support these 131,180 LTC-eligible HC clients was $1.3B, compared to the $4B spent for the care of approximately 100,000 Ontarians in its LTC homes.
Recently, the Ontario government more than doubled its construction funding subsidies from an average of $240 to $560K per bed, or $14 to $34B overall, to help further incentivize and accelerate the building of new and renovated LTC beds to meet its 2028 goal. However, it remains uncertain how this government’s goals will be met within its second mandate to help address its immediate and ongoing hallway medicine and waitlist pressures, especially given that currently only 1,934 new or renovated beds have been opened while only another 5,071 have begun construction during the last five years.
By assisting more LTC-eligible Ontarians to remain at home longer, with improved HC options, Ontario’s MHLTC could help to further encourage individuals and their families to defer or even avoid unwanted LTC home placements, further improving issues of hallway medicine, surgical backlogs and wait times.
Our Proposed Solution: The Virtual LTC @ Home Program
We are proposing that Canada undertake a major reorientation from its current prioritization of the provision of care in LTC homes to instead provide care within the homes and communities of Canadians with the implementation of a Virtual LTC @ Home Program.
This program would leverage existing infrastructure – people’s own beds in their homes, and existing community-based care providers – in new and innovative ways to offer LTC-eligible individuals (e.g., individuals already on or eligible to be added to an LTC home waitlist) the option to receive LTC home equivalent care in their own home through the creation of highly coordinated and integrated teams of care providers. These teams would need to bring together several key partners that can be found in most Canadian communities. For example, within each of Ontario’s emerging OHTs:
■ Local Community Support Services Agencies provide a core basket of services, including transportation, Meals on Wheels, adult day programs, and friendly visiting services, which enhance the overall well-being and social connectedness of participants.
■ HC Service Providers deliver professional services, including nursing, physiotherapy, occupational therapy, and personal support worker-led care that are essential to enabling people to live at home
■ Primary Care Providers play a pivotal role in coordinating a patient’s overall healthcare needs and ensure that individuals receive proper medical assessments, treatment plans, and ongoing monitoring.
■ Community Paramedics can offer 24/7 remote patient monitoring capabilities, enabling early identification of health issues and timely interventions. Their scheduled and non-scheduled home visits could further enhance clinical care, providing critical support to patients with complex health conditions.
Furthermore, existing local LTC homes could play a crucial role in supporting this alternative form of LTC by partnering with Virtual LTC @ Home Programs to provide a base for locally-delivered home and community-based care that could better support individuals on their waitlists. This could allow Virtual LTC clients to potentially never need to move into a LTC home while also promoting an opportunity for more seamless transitions from the community to LTC homes for other clients when required.
Potential Benefits and Cost Savings of a Virtual LTC @ Home Program
The Virtual LTC @ Home Program presents a promising opportunity to empower individuals and their families, save costs, and promote greater independence through the provision of more client-centered, cost-effective and high-quality care and services.
By being able to provide 24/7 remote monitoring of vital signs, this program can ensure that individuals receive highly proactive, preventative and connected care in the comfort of their homes enabled by community paramedics.
Personalized alerts and timely responses to health changes can allow for earlier interventions, reducing the likelihood of 911 calls, ED visits and hospitalizations.Moreover, the availability of video, home and clinic-based assessments, advice, and treatments in collaboration with primary care physicians can ensure that participants receive more comprehensive and tailored healthcare support. Improved access to community-based supports can prevent social isolation and better address the unique needs of each participant to promote their overall well-being and quality of life.
By offering a robust alternative option that enables ageing in one’s own home with more adequate support, this program can better provide more LTC-eligible individuals and their families with a greater sense of autonomy and control. This approach would not only enhance patient, family and provider experiences but also further optimize the allocation of resources for individuals with higher care needs.
As Ontario’s cost of building and redeveloping its planned LTC beds continues to reach a record-high $34B, transitioning more individuals from needing LTC home admissions to the care of Virtual LTC @ Home Programs will likely avoid the need for significant future capital expenses. Indeed, this program essentially would enable the government to allocate resources more efficiently, directing funds towards the provision of more effective in-home care, which has been proven to be more cost-effective than traditional LTC home-based care. Beyond significant saving from not having to build more care infrastructure, additional significant cost savings can be realized like they have been in the United States and Denmark through the delivery of more comprehensive home and community-based care solutions.
For example, instead of allocating funds to more of the same, it would be more beneficial for the province to invest in enhancing home and community care services – especially since according to
the MHLTC it costs around $750 per day to care for an ALC patient waiting for LTC in the hospital, while LTC home-based care costs around $200 per day, and HC for an LTC-eligible person is only $103 per day. This not only saves costs but also ensures that individuals can receive care in familiar surroundings (i.e., with or close to their own families), which can significantly and positively impact their overall well-being and quality of life.
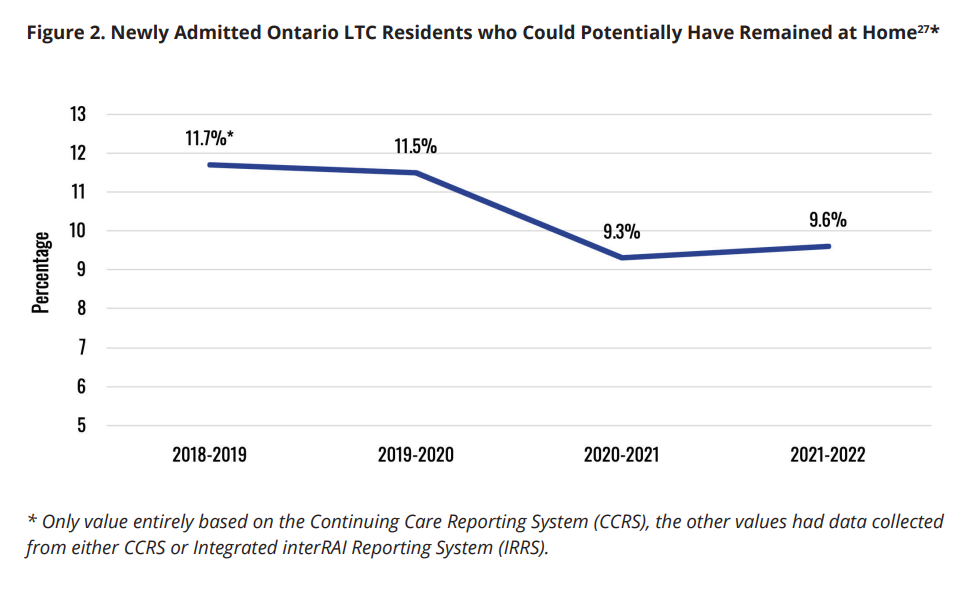
The Virtual LTC @ Home Program can also play a vital role in further alleviating the growing burdens on hospital and LTC beds, addressing the growing challenge of hallway healthcare. Studies have indicated that approximately 10% of Canadian LTC home residents may not require care in an LTC home, and with more properly organized supports could likely have remained in the community, further contributing to cost savings (see Figure 2). By leveraging local municipally administered community paramedic programs, this program can further reduce emergency calls and prevent avoidable hospital admissions. This proactive approach not only optimizes bed utilization but also enhances both patient and provider outcomes and experiences.
International Evidence and Success Stories to Support the Creation of a Virtual LTC @ Home Program
Our proposal to establish a Virtual LTC @ Home Program first in Ontario and then across Canada is informed by the significant international evidence that has emerged from countries like the United States and Denmark which have developed more robust HC programs similar to what is proposed here to successfully address their prior issues of hallway medicine and an unnecessary over reliance on institutional care.
Across Ontario and the rest of Canada, the current allocation of its overall LTC spending stood at $13.8B and $41.6B respectively in 2022-23 which focused 64% and 69% of its spending on providing care in institutional settings like hospitals and LTC homes (Table 1).
Table 1 also shows how over the past decade it has been one of the few jurisdictions in Canada whose increased spending on institutional-based LTC surpassed spending on home and community-based LTC services.
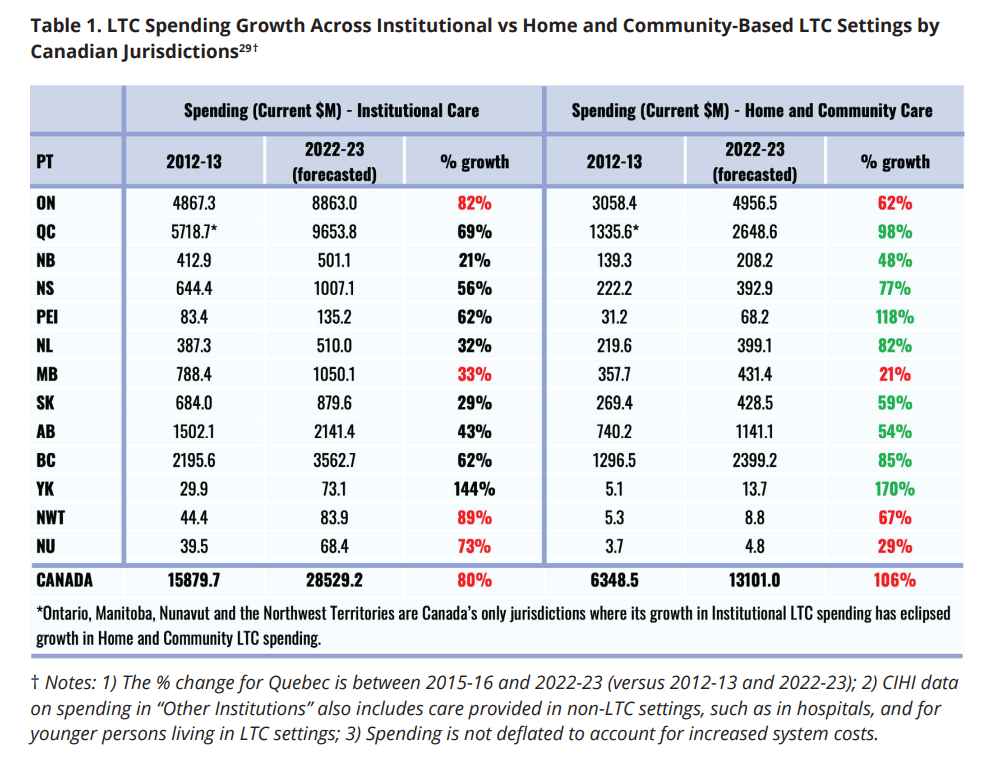
In contrast, Denmark, which has been championing its progressive Ageing-in-Place Strategy since 1988, now allocates only 36% of its overall LTC spending to care for individuals in LTC homes.
As a result, Denmark has achieved a current hospital-ALC rate of close to 1% compared to Ontario’s rate of 13.6%. Denmark also avoided building any additional LTC beds over two decades and closed thousands of hospital beds as a result of its strategy.
Furthermore, in the United States, its innovative Program for All-Inclusive Care for Elders (PACE) currently supports approximately 51,000 individuals 55 years and older who are LTC-eligible to live safely in the community with the support of one of 260 PACE programs across 31 states. These programs receive the equivalent funding amount per enrollee as would be given to care for them in LTC homes.
The PACE model offers a comprehensive continuum of medical care and long-term services for frail older adults, including primary and specialty medical care, inhome services, audiology, dentistry, optometry, podiatry, speech therapy, respite care, transportation, and adult day services. As a result, PACE enrollees experience fewer emergency department visits, a 24% lower hospitalization rate, and a 16% lower re-hospitalization rate compared to similar non-PACE clients.
Additionally, PACE participants have a reduced risk of eventually being admitted to LTC homes, and the program is found to alleviate family caregiver burden and provide support to improve family caregiving. One study found that only 15% of PACE enrollees eventually transitioned to living in LTC homes after three-years of enrollment.
Implementation Considerations
In advance of the 2022 election, the Ontario government announced that it would invest an additional $1B more over three years to provide more home and community care. In Budget 2023, it agreed to accelerate its commitment by injecting an extra $569 million solely for the provision of more home and community care during the 2023-24 fiscal year.
To help people realize that what we are proposing is evidence-informed, feasible and within our capacity to actually achieve the same transformative results as elsewhere, we are thus proposing that instead of doing more of the same, Ontario’s MHLTC should use a small proportion of its new home and community care investments to launch up to 10 Virtual LTC @ Home Demonstration Programs.
These programs could support up to 150 clients per year with up to $67,510 per enrollee (the current annual per-resident cost to provide a year of care in an Ontario LTC home), per year for an initial three-year period of funding. This would represent an investment of $100M a year, as part of Ontario’s $14B LTC services budget, to test our evidence-informed solution that could begin to finally put an end to Ontario’s debilitating hallway medicine and waitlist crisis once and for all.
In practice, there are several OHTs that have been established or are in development across the province that have the potential to become natural leaders for implementing a Virtual LTC @ Home Program. In fact, a majority of OHTs have already indicated that one of their core priorities is to promote better collaborations around the care of frail older adults in their communities, thus providing ripe environments to test such a program.
Ideally, an OHT, which includes many of the key providers outlined above, can self-organize to form the core elements needed to provide flexible, responsive 24/7 clinical service that complements standard care.
These integrated teams of care providers would have to collaborate to identify local individuals on LTC home waitlists who are not only eligible but would also prefer to stay at home for as long as possible and work to develop coordinated care plans tailored to each person’s evolving and immediate needs.
If this model and approach proves successful and gains popularity as a key alternative to LTC home placements, it may enable the Ontario MHLTC to establish more Virtual LTC @ Home Program “beds” within the government’s current mandate, and even allow it to forgo having to build or redevelop some of the 60,000 physical LTC beds its already struggling to bring online for potentially as much as $34B.
Beyond Ontario, Virtual LTC @ Home Programs could also be implemented nation-wide, like the PACE model in the US, as a proven solution to address worsening issues of hallway medicine, surgical backlogs and unprecedented ALC rates across the country. Such efforts are also consistent with the evolving preferences and values of all Canadians, especially concerning their current and future desire to age in their own homes and communities for as long as possible.
Conclusion
Given estimates that Canada will need to more than double it current complement of LTC beds by 2035 to meet the needs of its ageing population, the proposed Virtual LTC @ Home Program offers a high-impact, cost-effective, and politically desirable policy alternative to building more LTC homes that can effectively address health care wait times and other health care delivery challenges.
Offering dedicated funding for teams of local care providers to flexibly deliver a mix of care and support services, will allow more LTC-eligible individuals to live in their own homes longer, will reduce the need for LTC home admissions.
There will always be a role for LTC homes, and this program can ensure they are only used if needed by prioritizing the more appropriate provision of home and community care supports. In light of the compelling evidence and potential benefits presented in this proposal, we urge Ontario and Canadian policymakers and stakeholders to take bold action and implement the proposed Virtual LTC @ Home Program paving the way towards a more person-centred and sustainable future for the provision of healthcare and LTC services.
Acknowledgement
We would like to acknowledge the advice and mentorship provided by Dr. Samir K. Sinha MD, DPhil, FRCPC, Director of Health Policy Research, National Institute on Ageing, Toronto Metropolitan University and Director of Geriatrics, Sinai Health System and University Health Network in the creation and development of our proposal.
Read the proposal in PDF form:
Recommended for You

Ginny Roth: J.D. Vance, Pierre Poilievre, and how they slice their economic pie

David Polansky: As President Biden leaves the race, will the Democratic Party hodgepodge hold?

Peter Menzies: The mainstream media should love Doug Ford, now that he’s subsidizing them

Geoff Russ: A future Conservative government must fight the culture war, not stand idly by









